The Tipping Point for Digital Therapeutics is Here
The DTx adoption tipping point is closer than payers and the broader healthcare industry may realize. In the wake of the COVID-19 crisis, the pace of digital health transformation is accelerating on a massive scale.
4 min read

Further Reading
-
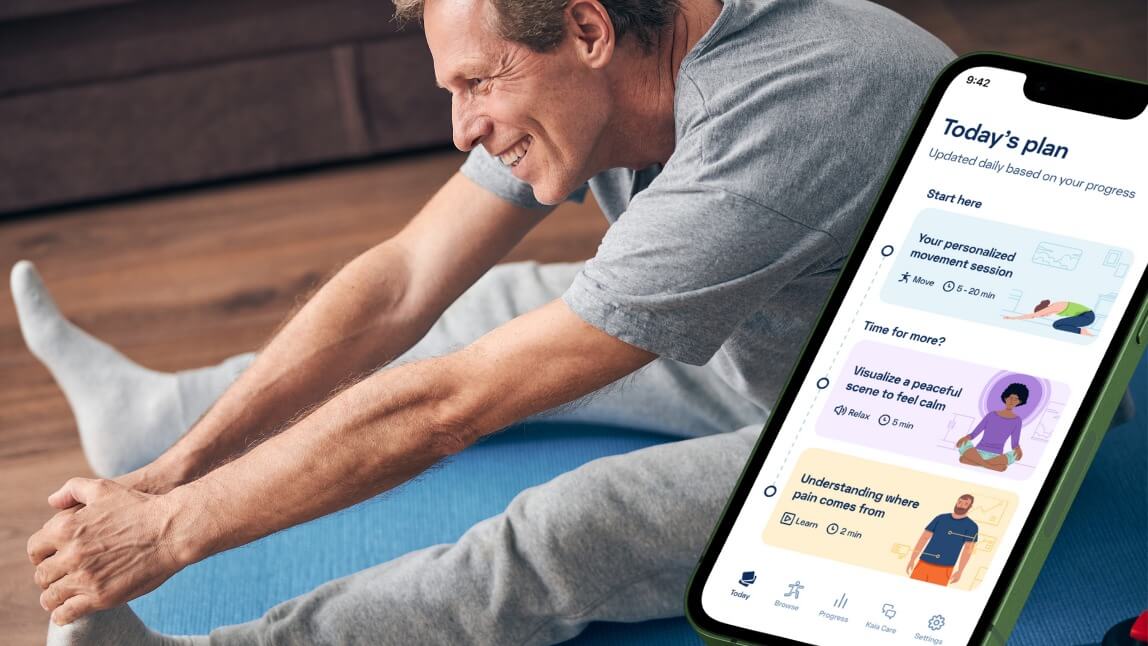
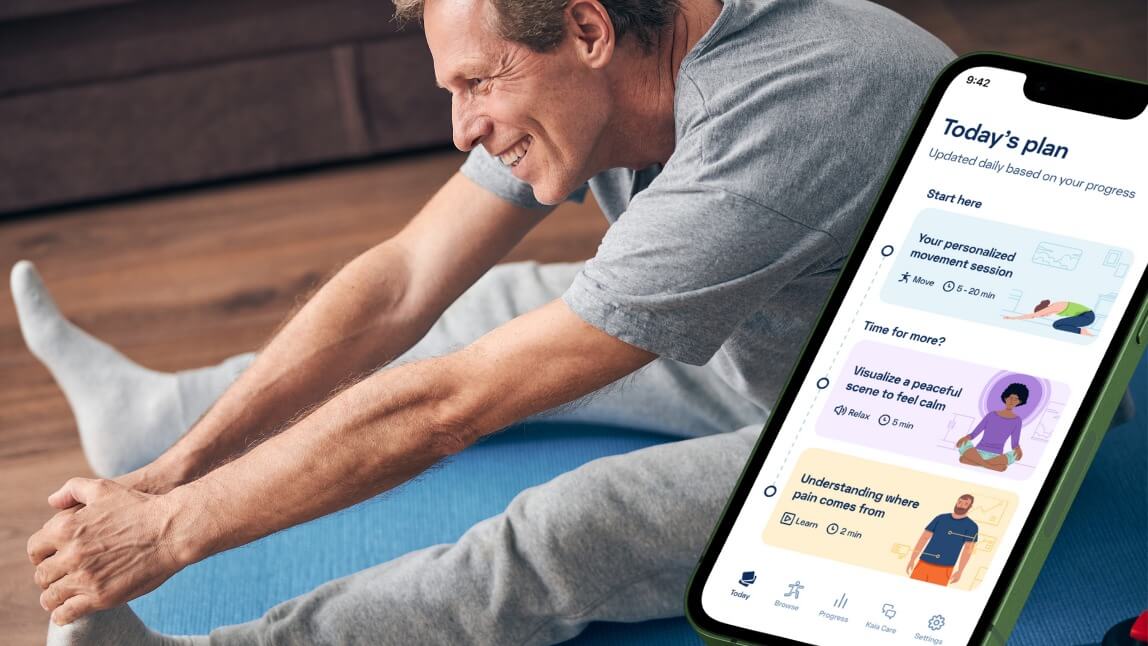 Find out how Kaia Health's digital-first, multimodal solution can help address musculoskeletal (MSK) pain and enhance employee well-being.3 min read
Find out how Kaia Health's digital-first, multimodal solution can help address musculoskeletal (MSK) pain and enhance employee well-being.3 min read -

Employee Health Access and Delivery in the New Normal
How HR and benefit leaders can prepare for COVID-19 challenges ahead.3 min read -

Place Your Bet on Engagement and ROI Will Follow
How to leverage digital health and personalization to manage chronic disease, improve population health and boost bottom-line results.3 min read