
What You Need to Know About Pelvic Floor Health
Expert Advice from a Certified Kaia Coach

Are you struggling with urinary or bowel incontinence, pelvic pain, or constipation? Then you might be suffering from pelvic floor dysfunction (PFD), and it’s nothing to be ashamed of. In fact, 25% of women in the United States will experience one or more symptoms of PFD in their lifetime and reports reveal that most will never seek the treatment they need.
To spread awareness and education, break the stigma surrounding this disorder, and improve access to care, we sat down with Courtney Mills, NBC-HWC, CIC, CPT, and Senior Health Coach at Kaia to hear about her experiences with PFD – both personally and professionally.
What is the pelvic floor and why is it important to keep it healthy?
“The pelvic floor is a group of muscles that run from the pubic bone to the tailbone. What I’ve discovered in my experience with pelvic floor dysfunction, is that we often take for granted the way our body gracefully moves through daily activities.
We use our pelvic floor constantly throughout the day – using the restroom, coughing, sneezing, doing chores, walking, running etc. We are unconsciously relaxing and activating our pelvic floor when needed, and only with the loss of these functions do we realize how vital they are to our physical, emotional, and mental well-being.”
What are the symptoms of a pelvic floor disorder?
“There are so many different symptoms people can experience related to the pelvic floor and rather than speak to the clinical side, I will mention my own experiences here.
During pregnancy I experienced sharp pain, sometimes radiating from my pubic bone. It usually began as a dull ache and as I stood and walked throughout the day, it would become more pronounced, with sharp pains that often took my breath away.
I also experienced severe urinary leakage postpartum with almost any activities that taxed the core and pelvic floor muscles (coughing, sneezing, jumping/running, baby wearing). There was a general feeling of fullness in my entire pelvic floor area, and I experienced more frequent constipation as well.”
How did pregnancy, postpartum, and perimenopause impact your pelvic floor health?
“Pregnancy was very challenging on my body. While I carried small (as a tall person), the impact my daughter had on my pelvic floor was tremendous. The entire last trimester I experienced dull, sharp, and shooting pain, as well as difficulty walking and discomfort using the restroom. Initially the pain was almost debilitating and I was no longer able to exercise at the level I was used to.
Postpartum, it turned into issues with urinary leakage, constipation and pelvic fullness. I was incredibly uncomfortable as I had a 2nd/3rd degree tear during birth. And so my sexual health was non-existent. As my hormones adjusted, I began to experience less pain but severe issues with urinary leakage and a worsening of constipation, something I experienced late pregnancy as well.
I also had what was considered to be a sensitive/reactive baby. She cried loudly and often and hated sleeping in the bassinet. I either wore her or strolled her for all her naps until she was close to a year old. As she got bigger, the baby wearing started to tax my pelvic floor and make my urinary issues worse. It all came to a head when my daughter started daycare and brought home sickness after sickness. I would cough and sneeze and my pelvic floor didn’t have the endurance to withstand it so I started having to wear liners and pads all the time.
Immediately after the postpartum period, I began experiencing perimenopausal symptoms, which can exacerbate existing pelvic floor issues because of the lack of estrogen, and changes in the vaginal and bladder tissues. Talk about a triple whammy.
I know everyone will have different experiences but what I’ve learned is that pelvic floor health is incredibly important at all stages and it is NEVER too late to improve symptoms.”
"Pelvic floor health is incredibly important at all stages and it is NEVER too late to improve symptoms."

When did you decide to reach out for help?
“Dealing with postpartum depression, I felt deeply betrayed by my own body. I’d been athletic my entire life, injury after injury, and nothing had held me back. I always bounced back. But not this time. It was getting worse and worse.
It was after the fifth or sixth illness that I reached out to one of Kaia’s internal Physical Therapists (PT), and good friend of mine, in tears. I needed help, and we spent a long conversation detailing my symptoms, feelings, and thoughts. She was the angel I needed during an incredibly challenging time. And with her expertise and compassion, we found a PT that was just right for me, and they changed my life!”
What are the barriers that prevent women from seeking help for PFDs and how can we address them?
Stigma and shame
“I believe a core issue around seeking help for pelvic health is shame or embarrassment. While the individual tends to carry this shame as their own, it’s not REALLY theirs.
It’s been my experience that we tend to avoid discussions around sex and genitalia as a society, and it’s often taboo to speak honestly and openly about our experiences. It is absolutely necessary to speak out about the issues we experience and consequently, the lack of care we receive. It’s the only way to normalize them as an inevitability of childbirth or aging.
I cannot even begin to express the anger I feel when a fellow mom jokes about urinary leakage being part of motherhood. NO IT IS NOT!!! We do not have to accept the way things have always been simply because it’s uncomfortable to challenge the status quo.
Additionally, there is an overwhelming emphasis on the well-being of the new baby postpartum but I don’t think that same concern exists for the new mother. A single check up six weeks postpartum is often the only care a mother receives and in a culture that tends to encourage women to focus on the baby, it can lead to a woman to neglect the symptoms she is experiencing.”
Lack of access to education and care
“There is a lack of access many individuals have as well. I was able to see an amazing professional for in-person PT but it was after a terrible first experience. I imagine many folks echo a story of sub-optimal care and unfortunately, one negative experience can scare so many people from trying again.
The PT I ended up with specialized in pelvic floor work which means she was SUPERB, but very expensive. Insurance doesn’t support coverage for many of these specialty providers which will greatly impact the number of women who can seek treatment. This is also why Kaia Health can be a fantastic alternative to in-person care.
I also believe educating all health professionals, regardless of speciality, around basic pelvic floor health and the proper channels to refer patients to would open many doors as well. There is nothing worse for a patient than having the courage to speak up, only to be referred to the wrong place, or told that these experiences are a normal consequence of childbirth, aging etc.”
"We do not have to accept the way things have always been simply because it's uncomfortable to challenge the status quo."
Tell us about the pelvic floor support offered by Kaia Health?
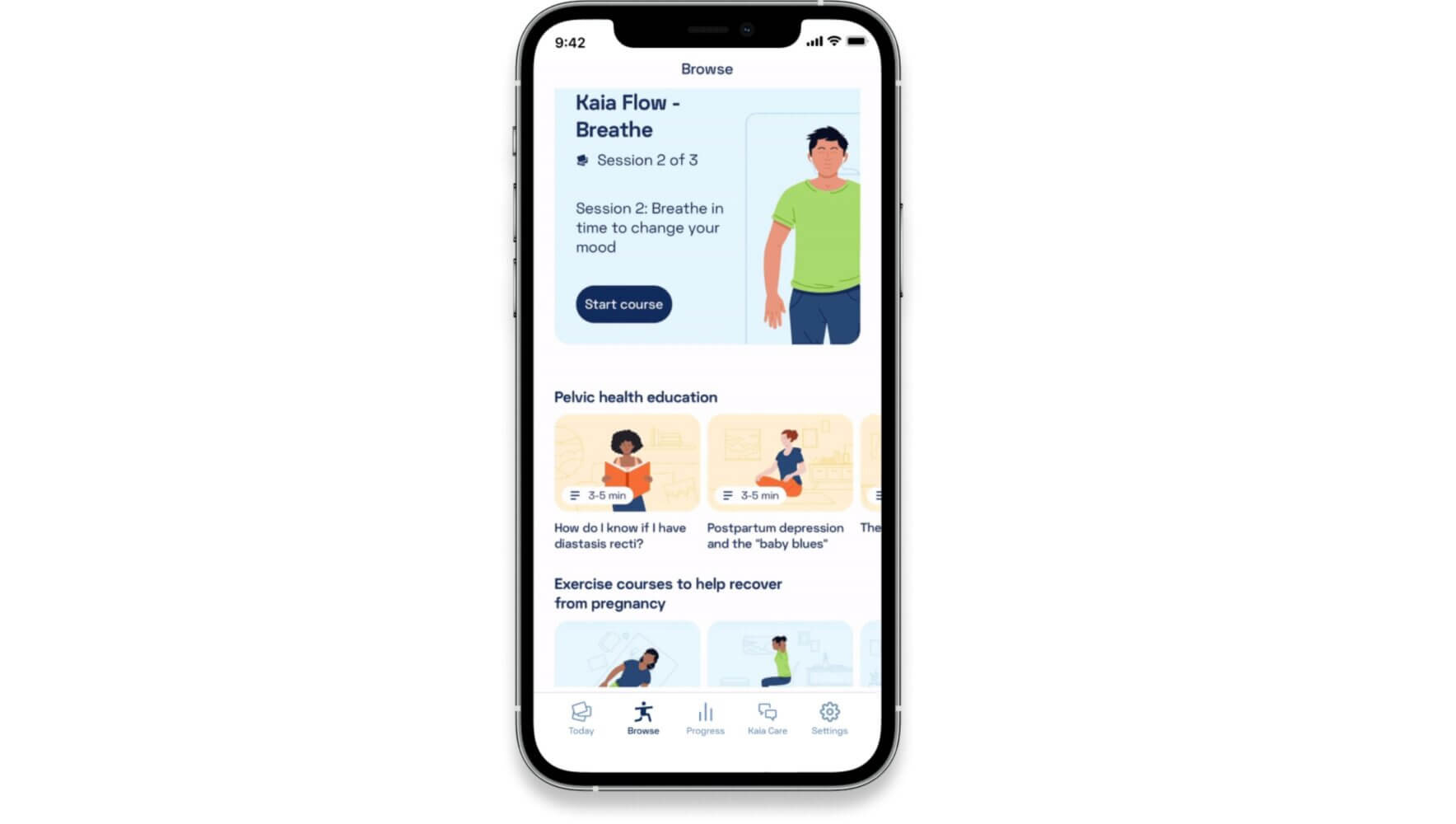
“The Kaia app offers an incredible source of education to women suffering from symptoms of PFDs. You can learn about breathing (a key pillar in pelvic floor work) as well as different aspects of pain, bladder/bowel issues, and the postpartum period. Kaia’s in-app support provides a wonderful opportunity to gain a better understanding of your body, and the importance of a healthy pelvic floor that women can take with them for the rest of their lives.
In-app exercises provide a solid foundation to build a pelvic floor that can operate optimally. There is so much information out there. A great deal of information focuses on kegels. But sometimes this isn’t what is needed for the individual. In my case, I had an overactive pelvic floor so strength wasn’t my main issue and kegels were not the cornerstone of my program.
Kaia’s therapy focuses on the whole person, providing gentle exercises that are safe and focusing on integrating breath work with movement and stretches. There is also an emphasis on learning how to breathe with the pelvic floor during movement. This is key in making improvements.”
What differentiates Kaia from other solutions on the market?
“I think what separates us from other options is that we provide each individual with the opportunity to access pelvic floor support in the comfort of their home, with the autonomy and flexibility to integrate it into their life in a way that works for them. Our team of PTs developed the therapy with safety, efficacy, and empathy at the heart of every exercise and educational offering.
Our team cares and it’s evident by the attention and sensitivity with which they approached this specific therapy. We also offer coaching (I’m one of the coaches btw – hi!) so if users run into challenges or have questions, they can connect with someone that wants to help. One of the biggest challenges of any physical therapy program is staying compliant and being consistent over a period of time in order to see results. We can help!
As a final note to anyone reading this, my hope is that if you take away anything, it’s that it is NEVER TOO LATE to feel better. You can feel better and, most importantly, you deserve it.”

About Courtney Mills
Courtney is a Senior Health Coach with Kaia Health who is passionate about helping people realize their potential, reach their health goals, and fall in love with the process. She’s been in the health and wellness space for over 20 years and has worked with nearly every demographic, at every phase in life. In her spare time, she enjoys baking, taking walks with family, listening to “every podcast under the sun,” and dancing. Her personal journey through a difficult pregnancy and postpartum period inspired her to advocate for awareness and recovery regarding pelvic floor issues, sharing her own experiences to encourage and support others.
“Now, a year later, I continue to surpass my goals of feeling more like myself with fewer pelvic floor issues, and want to inspire and encourage others to start their own journey toward feeling better.”
Learn more about how Kaia Health is enhancing access to women’s healthcare nationwide with clinically-validated, pelvic floor support, here.
Further Reading
-
 Here are six easy exercises for back pain you can do in just minutes a day to prevent, reduce, and relieve work-related back pain.3 min read
Here are six easy exercises for back pain you can do in just minutes a day to prevent, reduce, and relieve work-related back pain.3 min read -

Five Exercises to Relieve Lower Back Pain
Find fast relief from lower back pain with easy exercises and stretches you can do from the comfort of your home.4 min read -

Q&A with Simon Hayhurst, Chief Product Officer
A peek behind the curtain to see how Angela, Kaia’s AI-powered digital care assistant, came to life.4 min read